Adult Aquired FlatFoot Causes
Overview Another common term for this condition is Posterior Tibial Tendon Dysfunction (PTTD). There is a cause-effect relationship between pronation, flatfoot deformity and subsequent tenosynovitis of the posterior tibial tendon. Mechanical irritation of the tendon may lead to synovitis, partial tearing and eventually full rupture of the tendon. Other structures, including ligaments and the plantar fascia, have also been shown to contribute to the arch collapsing. As the deformity progresses, these structures have been shown to attenuate and rupture as well. In later stages, subluxation of various joints lead to a valgus rearfoot and transverse plane deformity of the forefoot. These deformities can become fixed and irreducible as significant osteoarthritis sets in.  Causes Women are affected by Adult Acquired Flatfoot four times more frequently than men. Adult Flatfoot generally occurs in middle to older age people. Most people who acquire the condition already have flat feet. One arch begins to flatten more, then pain and swelling develop on the inside of the ankle. This condition generally affects only one foot. It is unclear why women are affected more often than men. But factors that may increase your risk of Adult Flatfoot include diabetes, hypertension, and obesity. Symptoms Pain and swelling around the inside aspect of the ankle initially. Later, the arch of the foot may fall (foot becomes flat), this change leads to walking to become difficult and painful, as well as standing for long periods. As the flat foot becomes established, pain may progress to the outer part of the ankle. Eventually, arthritis may develop. Diagnosis The history and physical examination are probably the most important tools the physician uses to diagnose this problem. The wear pattern on your shoes can offer some helpful clues. Muscle testing helps identify any areas of weakness or muscle impairment. This should be done in both the weight bearing and nonweight bearing positions. A very effective test is the single heel raise. You will be asked to stand on one foot and rise up on your toes. You should be able to lift your heel off the ground easily while keeping the calcaneus (heel bone) in the middle with slight inversion (turned inward). X-rays are often used to study the position, shape, and alignment of the bones in the feet and ankles. Magnetic resonance (MR) imaging is the imaging modality of choice for evaluating the posterior tibial tendon and spring ligament complex. Non surgical Treatment Nonoperative therapy for adult-acquired flatfoot is a reasonable treatment option that is likely to be beneficial for most patients. In this article, we describe the results of a retrospective cohort study that focused on nonoperative measures, including bracing, physical therapy, and anti-inflammatory medications, used to treat adult-acquired flatfoot in 64 consecutive patients. The results revealed the incidence of successful nonsurgical treatment to be 87.5% (56 of 64 patients), over the 27-month observation period. Overall, 78.12% of the patients with adult-acquired flatfoot were obese (body mass index [BMI] = 30), and 62.5% of the patients who failed nonsurgical therapy were obese; however, logistic regression failed to show that BMI was statistically significantly associated with the outcome of treatment. The use of any form of bracing was statistically significantly associated with successful nonsurgical treatment (fully adjusted OR = 19.8621, 95% CI 1.8774 to 210.134), whereas the presence of a split-tear of the tibialis posterior on magnetic resonance image scans was statistically significantly associated with failed nonsurgical treatment (fully adjusted OR = 0.016, 95% CI 0.0011 to 0.2347). The results of this investigation indicate that a systematic nonsurgical treatment approach to the treatment of the adult-acquired flatfoot deformity can be successful in most cases.
Causes Women are affected by Adult Acquired Flatfoot four times more frequently than men. Adult Flatfoot generally occurs in middle to older age people. Most people who acquire the condition already have flat feet. One arch begins to flatten more, then pain and swelling develop on the inside of the ankle. This condition generally affects only one foot. It is unclear why women are affected more often than men. But factors that may increase your risk of Adult Flatfoot include diabetes, hypertension, and obesity. Symptoms Pain and swelling around the inside aspect of the ankle initially. Later, the arch of the foot may fall (foot becomes flat), this change leads to walking to become difficult and painful, as well as standing for long periods. As the flat foot becomes established, pain may progress to the outer part of the ankle. Eventually, arthritis may develop. Diagnosis The history and physical examination are probably the most important tools the physician uses to diagnose this problem. The wear pattern on your shoes can offer some helpful clues. Muscle testing helps identify any areas of weakness or muscle impairment. This should be done in both the weight bearing and nonweight bearing positions. A very effective test is the single heel raise. You will be asked to stand on one foot and rise up on your toes. You should be able to lift your heel off the ground easily while keeping the calcaneus (heel bone) in the middle with slight inversion (turned inward). X-rays are often used to study the position, shape, and alignment of the bones in the feet and ankles. Magnetic resonance (MR) imaging is the imaging modality of choice for evaluating the posterior tibial tendon and spring ligament complex. Non surgical Treatment Nonoperative therapy for adult-acquired flatfoot is a reasonable treatment option that is likely to be beneficial for most patients. In this article, we describe the results of a retrospective cohort study that focused on nonoperative measures, including bracing, physical therapy, and anti-inflammatory medications, used to treat adult-acquired flatfoot in 64 consecutive patients. The results revealed the incidence of successful nonsurgical treatment to be 87.5% (56 of 64 patients), over the 27-month observation period. Overall, 78.12% of the patients with adult-acquired flatfoot were obese (body mass index [BMI] = 30), and 62.5% of the patients who failed nonsurgical therapy were obese; however, logistic regression failed to show that BMI was statistically significantly associated with the outcome of treatment. The use of any form of bracing was statistically significantly associated with successful nonsurgical treatment (fully adjusted OR = 19.8621, 95% CI 1.8774 to 210.134), whereas the presence of a split-tear of the tibialis posterior on magnetic resonance image scans was statistically significantly associated with failed nonsurgical treatment (fully adjusted OR = 0.016, 95% CI 0.0011 to 0.2347). The results of this investigation indicate that a systematic nonsurgical treatment approach to the treatment of the adult-acquired flatfoot deformity can be successful in most cases. 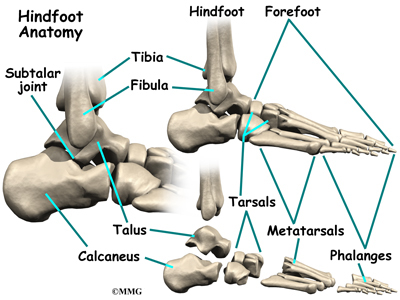 Surgical Treatment For those patients with PTTD that have severe deformity or have not improved with conservative treatments, surgery may be necessary to return them to daily activity. Surgery for PTTD may include repair of the diseased tendon and possible tendon transfer to a nearby healthy tendon, surgery on the surrounding bones or joints to prevent biomechanical abnormalities that may be a contributing factor or both.
Surgical Treatment For those patients with PTTD that have severe deformity or have not improved with conservative treatments, surgery may be necessary to return them to daily activity. Surgery for PTTD may include repair of the diseased tendon and possible tendon transfer to a nearby healthy tendon, surgery on the surrounding bones or joints to prevent biomechanical abnormalities that may be a contributing factor or both.